Objective
To assess the efficacy and safety of a “mini-perc” technique of percutaneous nephrolithotomy using a 14-Fr peel-away sheath for the removal of pyelocaliceal stones, and to determine appropriate inclusion criteria.
Materials and Methods
From July 1999 to June 2002, the medical records and radiographic images of 72 patients who underwent the “mini-perc” technique of percutaneous nephrolithotomy with a 14-Fr peel-away sheath, were reviewed to determine clinical history, stone characteristics, immediate stone free rate, final stone free rate after additional procedures, complications, and hospital stay. We also analyzed the effect of the longest stone diameter, the cumulative longest diameter of stones, the cumulative stone burden, and the stone density on the immediate stone free rate using a Fisher exact test.
Results
The only major complication, arterial bleeding, occurred in a patient with Child A liver cirrhosis and was successfully treated by embolization with coils and a gelatin sponge. The immediate stone free rate was 80.6%, which was significantly influenced by stone diameter but not stone density. The mean hospital stay after the procedure was 3.97 days.
Conclusion
The “mini-perc” technique of percutaneous nephrolithotomy, which uses the 14-Fr peel-away sheath, is a safe and effective modality for treating renal calculi.
In the early 1980’s, percutaneous nephrolithotomy replaced open surgery in a majority of renal stone treatments . However, it is frequently regarded as a second-line therapy for several reasons, including procedure-related hemorrhages requiring a blood transfusion or intervention , a greater demand for postoperative parenteral pain medication, and a longer hospital stay .
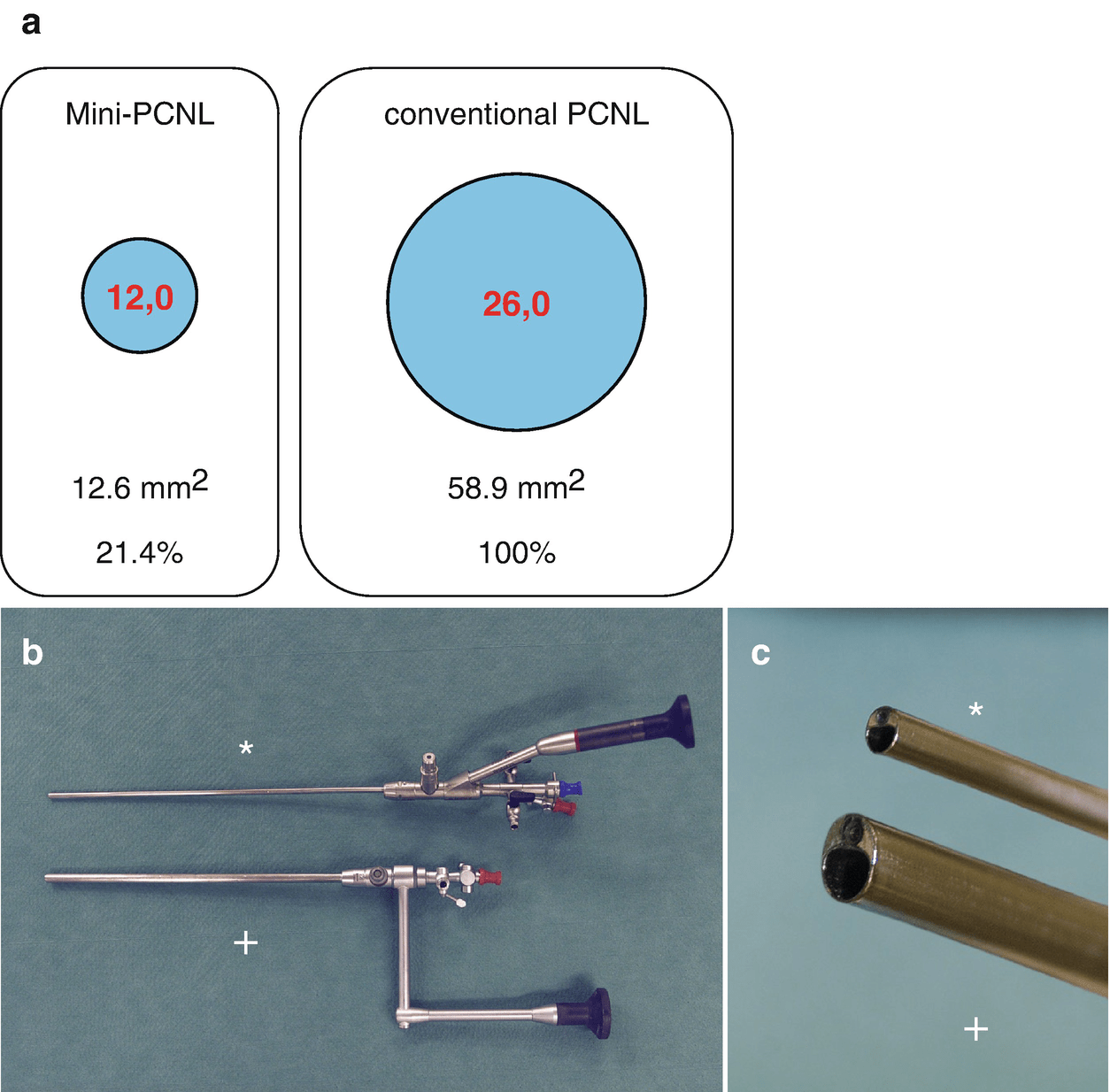
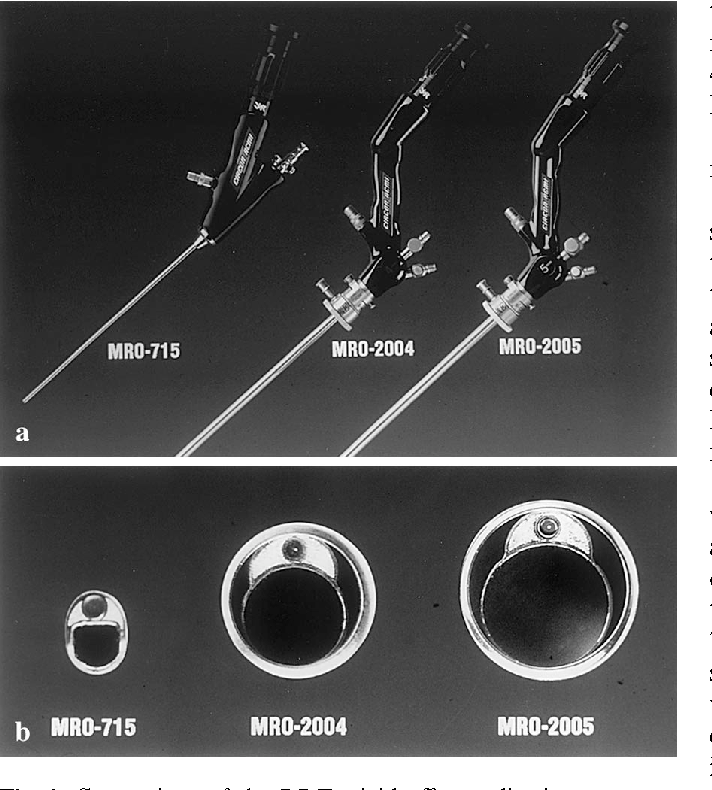
To reduce the disadvantages of conventional percutaneous nephrolithotomy, a “mini-perc” technique was first developed for children and reported by Helal et al. Additionally, Jackman et al. defined the “mini-perc” as a percutaneous nephrolithotomy achieved through a sheath too small to accommodate a standard rigid nephroscope. Other studies also described this technique as an effective and safe procedure . However, there have been no follow-up reports of experiences in a larger series.
The purpose of this study was to assess the safety and effectiveness of using a 14-Fr peel-away sheath for the removal of pyelocaliceal stones by reviewing our experience, as well as to determine the appropriate inclusion criteria.
MATERIALS AND METHODS
Patient Selection and Data Collection
During the 3-year period from July 1999 to June 2002, the “mini-perc” technique of percutaneous nephrolithotomy on pyelocaliceal stones was performed in 72 consecutive patients at our hospital. This study was approved by the Institutional Review Board, and written informed consent was obtained from each patient or their family members at the time of enrollment in the study, after the nature of the procedure and possible complications had been fully explained. There were 27 women and 45 men, and the age range was 1.4 years to 73 years (mean age, 49.5 years ± 14.7). The indications included failed shock wave lithotripsy and/or ureteroscopy in 19 subjects, a large cumulative stone burden (> 6 cm2) in 25, renal pelvis and/or lower pole calyceal stones in 62, upper calyceal stones in two, stone in calyceal diverticulum in one, and one child. Thirty-one of 72 patients had more than two of these indications.
Medical records of each patient were reviewed to determine the duration of symptoms, previous medical history, pre- and post-“mini-perc” interventional procedures, and hospital stay after the “mini-perc”. Radiologic examinations were also reviewed in all patients, including abdominal radiography, intravenous urography, antegrade pyelography, renal ultrasound, abdominal computed tomography, and abdominal magnetic resonance imaging.
Data on the stone number, location, longest stone diameter, the cumulative longest diameter of stones, cumulative stone burden, and stone density were also determined on a preoperative plain abdominal radiograph. The stone burden was defined as the two-dimensional area determined by multiplying the length by the width of the stone. Stone density was graded on three levels based on comparison with the adjacent rib (3: more dense, 2: isodense, 1: less dense). Postoperative evaluation of residual stones was done radiologically and nephroscopically. The immediate stone-free rate, complications after the “mini-perc”, and final stone-free rate after additional procedures were determined. We also assessed the effect of the longest stone diameter, the cumulative longest diameter, cumulative stone burden, and stone density on the immediate stone-free rate.
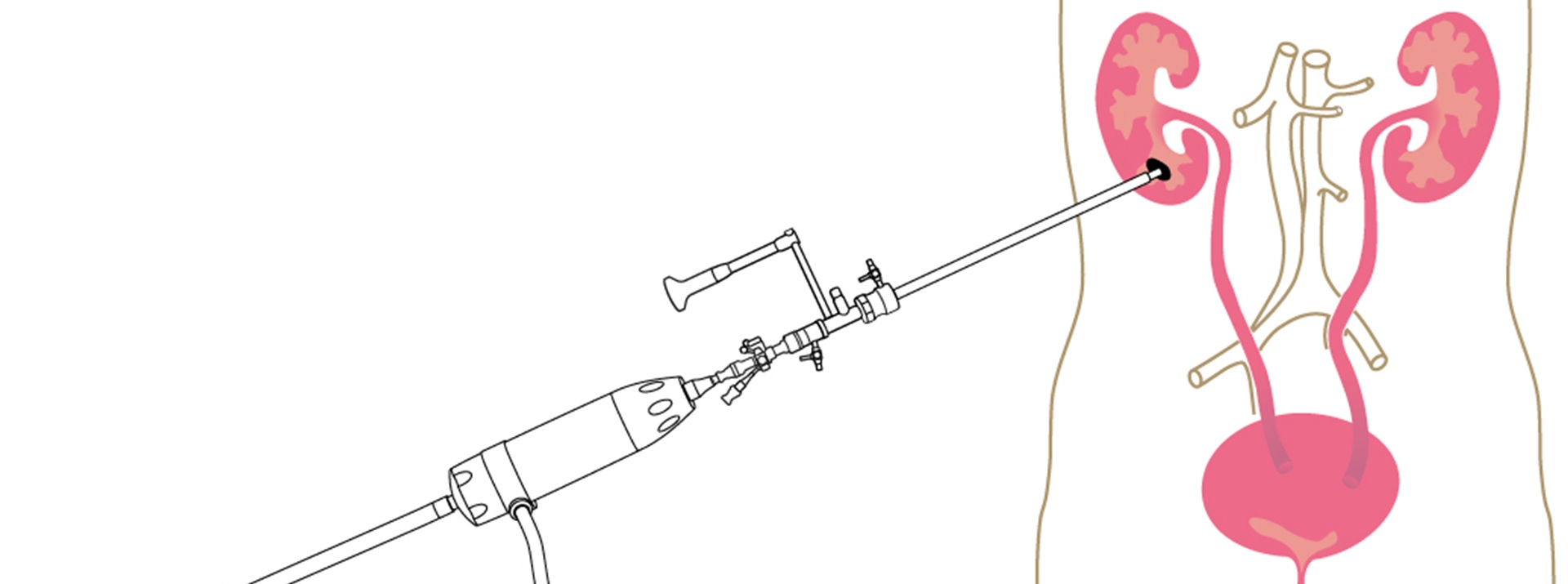
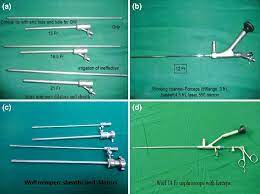
“Mini-Perc” Technique and Lithotripsy
Routine percutaneous renal access was performed in the interventional radiology suite on the day or one day prior to the planned “mini-perc”. Local anesthesia was used at the puncture site with the exception of a 17-month-old boy, who underwent general anesthesia . The definitive puncture was performed into the appropriate calyx with a 22-gauge Chiba needle (Cook, Bloomington, IL) under real-time ultrasound and fluoroscopic guidance. The approach most commonly was done through a lower pole calyx, or the postero-inferior aspect of the renal stones . The nephrostomy was created in an upper pole calyx in two patients who had upper calyceal stones. A 0.035-inch Radifocus guide wire (Terumo, Tokyo, Japan) was advanced through the nephrostomy tract into the bladder as a safety guide wire. An Amplatz Super Stiff guide wire (Boston Scientific, Miami, FL) was inserted into the bladder as a working guide wire . Nephrostomy tract dilation was then performed to the 14 Fr with serial dilators (Cook, Bloomington, IL), a 14-Fr peel-away sheath (Cook, Bloomington, IL) was advanced through the working guide wire.
